Science & Society #1 – The Opioid Epidemic

“It started after my surgery.”
“I was given a prescription following my dental procedure.”
“It was just a few pills in the beginning.”
If you’ve heard someone’s story about opioid addiction, it is quite possible that you’ve heard one of these statements. Many people tell a similar story – they became addicted to opioids following a medical intervention. Sadly, once addicted, it can be a difficult habit to break. In March 2018, the Centers for Disease Control and Prevention (CDC) published the most recent data (2016) related to overdose deaths caused by opioids, cocaine, and psychostimulants. More than two-thirds of the 63,632 drug overdose deaths in the U.S. during 2016 were related to opioid abuse. This represented an almost 28 percent increase over the previous year.
The CDC report discussed three waves in the current epidemic:
- The first began in the 1990s with opioid overdoses including those resulting from prescription drugs.
- A second wave, which centered on heroin overdoses, began in 2010.
- The third and current wave began in 2013. The wave was again caused by an abuse of synthetic opioids, such as fentanyl. This time, however, the abuse was caused by both prescribed and illegally produced versions.
These medications are all chemically related. Opium, morphine, heroin, codeine, oxycodone, and fentanyl were all originally derived from the opium poppy, a plant first described more than 6,000 years ago.1
Many blame the current epidemic on the over-prescription of opioid-based drugs by healthcare providers. Indeed, efforts to curtail this public health epidemic include education about and alteration of prescribing practices as well as research into the development of non-opioid–based pain relievers and alternative therapies.
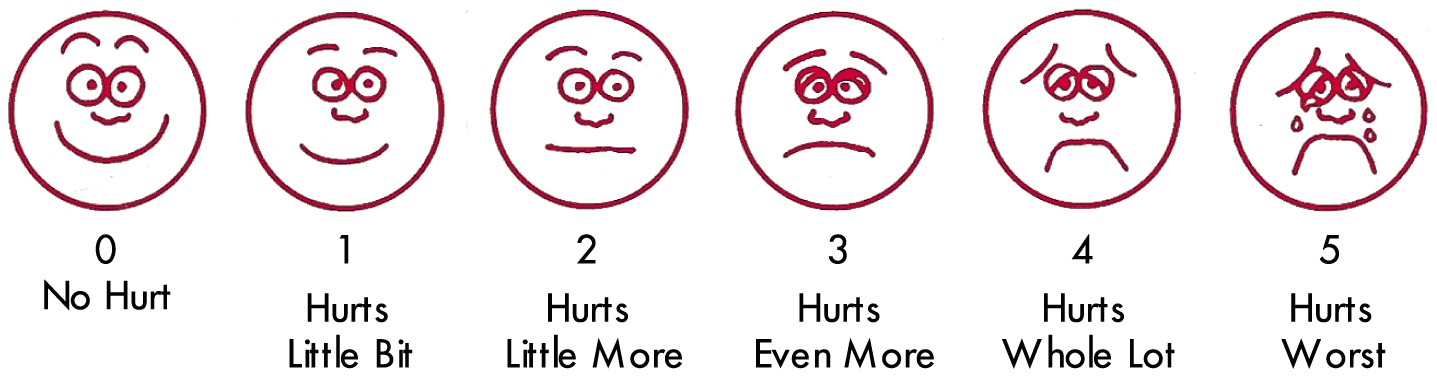
Clinicians definitely have to do better. But what is the role of the patient and the public? Specifically, how does pain tolerance fit into the equation? On one hand, doctors need to treat patients’ pain, but on the other hand, they must avoid contributing to the current epidemic. Pain is a subjective symptom. It is not something that can be measured, like blood pressure or temperature. Nor can it be observed, like a rash or flushed coloring. Medical personnel try to get a handle on a patient’s pain using pain rating systems based on numbers or images. But, even with those, how I rate my pain and how you rate the same pain may be very different.
For Discussion
When a person becomes a doctor, they often recite the Hippocratic Oath. The oft repeated part of that oath is “first do no harm.” So, where does the current epidemic fit when it comes to appropriately managing pain and inadvertently contributing to the current opioid epidemic?
Additional resources
1To find out more about the history and chemistry of opioids, check out Chapter 1, God’s Own Medicine, of Pandora’s Lab: Seven Stories of Science Gone Wrong, by Paul A. Offit, MD.
To find out more about drug overdoses in the U.S. over the last several decades, read this paper by Hawre Jalal, et. al., published in the journal Science on Sept. 21, 2018, Changing dynamics of the drug overdose epidemic in the United Sates from 1979 through 2016.
About the series
The Science & Society discussion series is based on the book, Pandora’s Lab: Seven Stories of Science Gone Wrong, by Dr. Paul Offit, Director of the Vaccine Education Center at Children’s Hospital of Philadelphia. We understand that teachers are using this book in high school classrooms, so in an effort to continue providing classroom resources, we developed this series to provide short reading passages that will leave students with questions to further explore in classroom discussions or specific projects. By presenting scientific ideas representing two sides of an issue, students will have the opportunity to consider how science fits into society from political, ethical, and legal points of view.